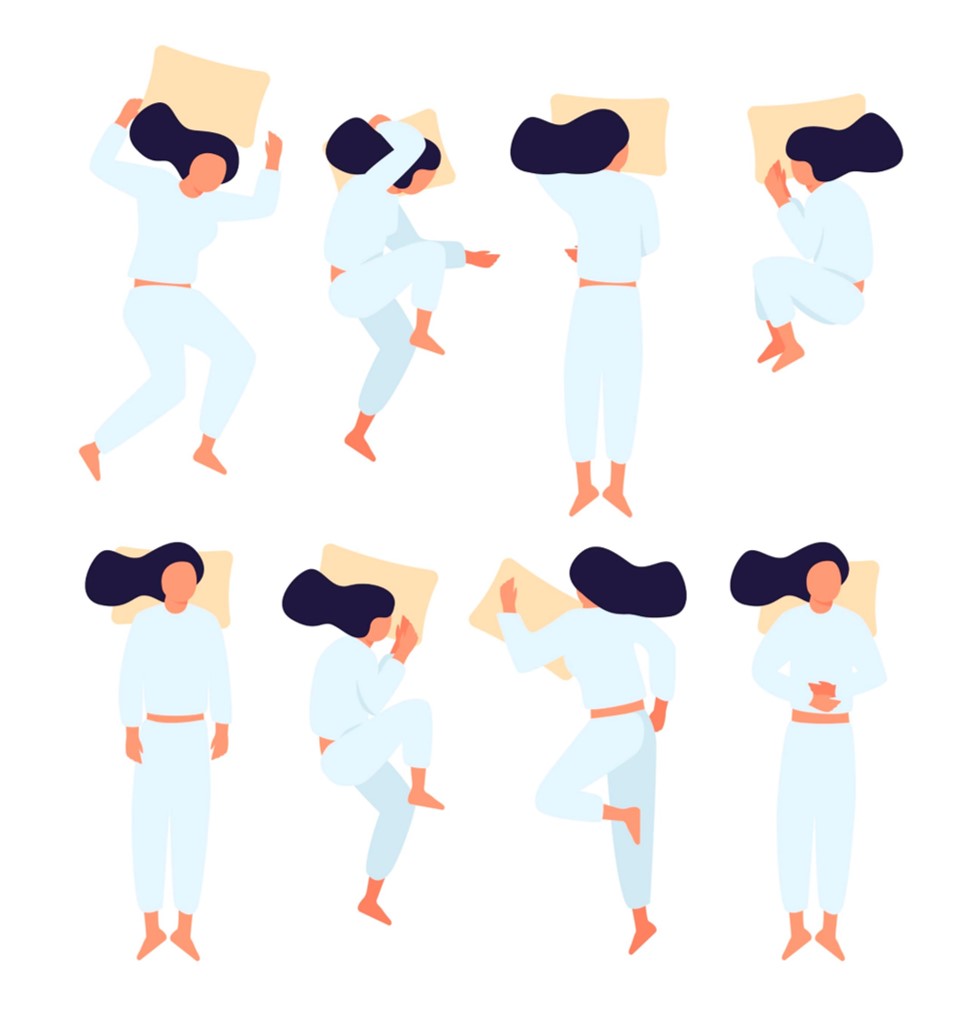
 If you’ve ever had a surgical procedure or medical condition that prevented you from sleeping in the position to which you’re accustomed, you might not have gotten much rest.
If you’ve ever had a surgical procedure or medical condition that prevented you from sleeping in the position to which you’re accustomed, you might not have gotten much rest.
Women recovering from a mastectomy are limited to only sleeping on their backs. A terrible cough might force you to sit upright, just to get some much-needed slumber. Pregnant women face all sorts of sleep position challenges.
Chronic snorers—whether due to sleep apnea or some other issue—are often relegated to side or stomach sleeping positions, sometimes forcibly so by a rib-poking bed partner.
What does your natural sleep position say about your health? Could a deviation from it indicate a deeper, underlying issue?
Apnea: Don’t Mess Around

According to the American Sleep Apnea Association, an estimated 22 million Americans suffer from sleep apnea, with the vast majority of cases still undiagnosed. Approximately 38,000 individuals die annually from heart disease directly complicated by apnea.
Countless others are impacted mentally and emotionally by the sheer fatigue apnea generates.
What is the best position for apnea sufferers?
Overall, sleep researchers claim the healthiest position for a healthy spine and proper alignment is on your back, with a pillow under your neck (not your head) so that your head is not forced forward.
Kathleen Gallagher, manager of the Riverside Sleep Disorder Institute, says such a recommendation doesn’t always apply. “For an individual who has issues with snoring and sleep apnea, the back is not the best position for sleep,” states Gallagher.
Unfortunately, as individuals enter the different stages of sleep, they may naturally gravitate to one position or another. For apnea sufferers, that could be a dangerous transition.
Gallagher advises undergoing a sleep study to determine if medical intervention such as a CPAP machine is necessary.
Changes in Sleep Behavior Provide Real-Life Clues
Fluctuating sleep positions may indicate more than just physical health challenges.
“If you’re sleeping with a partner, there might be some spooning, cuddling, or hugging. Or, maybe not. If you are somebody who has been very close to your bed partner and suddenly you’ve drifted apart, it might be time to think about what’s going on and why the abrupt disconnect,” says Gallagher. “That’s why I say sleep can tell a lot about what’s going on in your life—in the bedroom and outside of it.”
A Fancy Mattress Doesn’t Cure All
With all the advancements in sleep technology, mattresses have been a key component in improving nightly rest. Gallagher agrees—to a point. “We spend a third of our lives sleeping, so you really want to have something comfortable to sleep on.”
But, snoozing in a bed that adjusts to your unique needs doesn’t mean you have solved all your bedtime dilemmas. If you’ve replaced your mattress but still continue to wake up fatigued, like you just can’t get enough rest, it’s time to look at other potential culprits.
“When you go to bed, you shouldn’t be thinking about anything except sleep. That’s your quiet time, so really pay attention to how your body feels,” advises Gallagher. “Are you experiencing any new pains or aches? Do you have a scratchy throat or persistent cough? Anything that keeps you from your most restful sleep position can be a significant sleep interrupter.”
Of course, if you’re not sleeping—whatever the reason—you don’t have to suffer unnecessarily. Check-in with your primary care provider, who can prescribe a sleep study and get you on the path to healthier shuteye.
To listen to an interview with Kathleen Gallagher, manager of the Riverside Sleep Disorder Institute, click here.